What’s Up: The ICU Challenge – Obtaining a Clear ECG Signal on Critically ill Patients
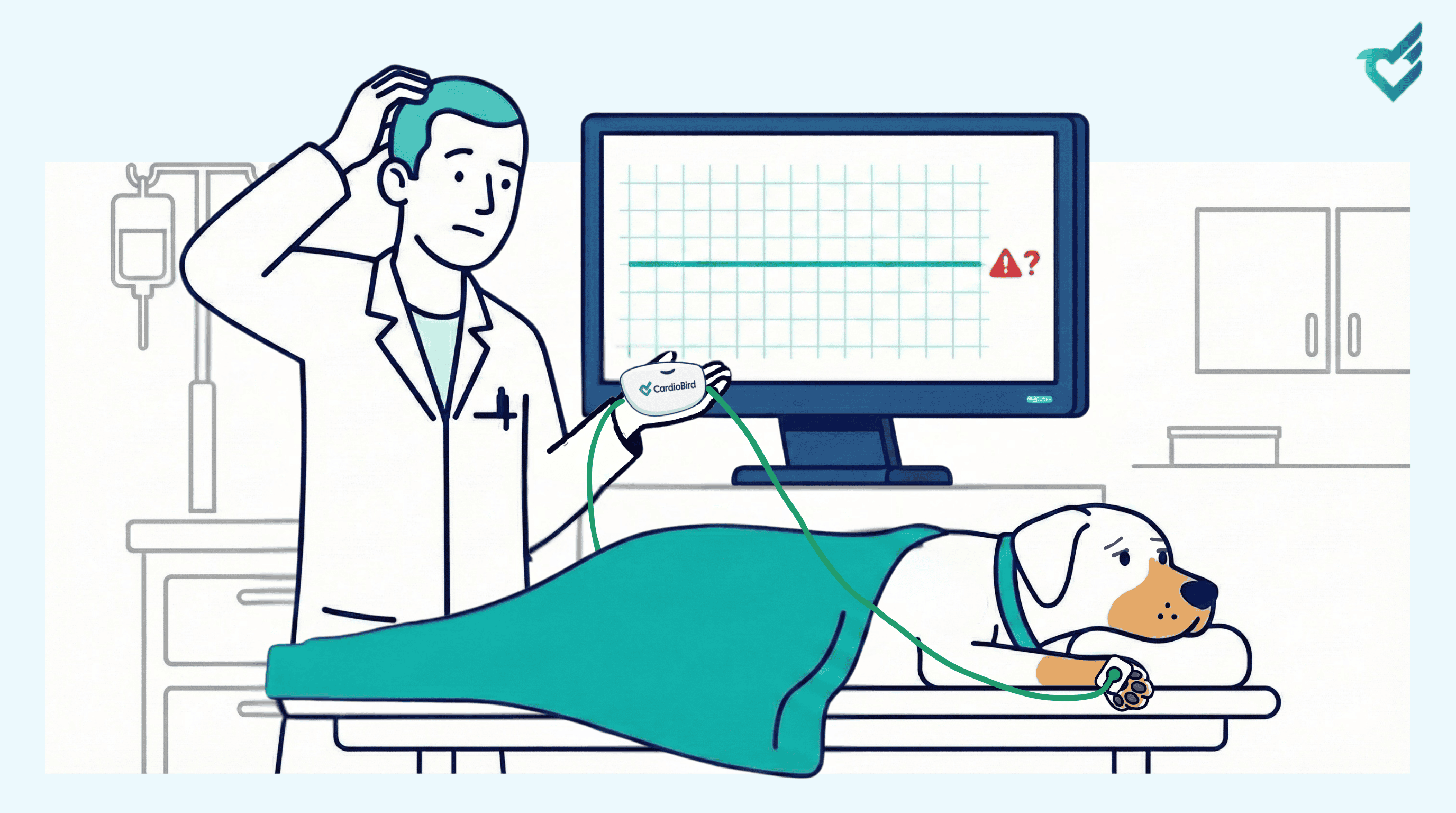
Welcome to a special technical edition of “What’s Up.” Many of you use CardioBird seamlessly for pre-anesthetic checks, routine exams, and continuous monitoring, where a clear ECG appears instantly after applying the electrodes to the limbs with metal clip or electrode pads on paws. However, in the Intensive Care Unit (ICU), you may encounter a frustrating scenario: connecting the leads to a critical patient only to see a flat line or a “lead off” alert. Why does this happen, and how can you overcome it?
This is a common, physiology-driven challenge, not a system failure. Successfully monitoring these vulnerable patients requires understanding the “why” and mastering the “how.”
Why the Signal Disappears: The Physiology of a Weak ECG
In the ICU, three key factors often converge to degrade or hide the heart’s electrical signal:
- Severely Low QRS Voltage: This is the prime suspect. The ECG measures the voltage of the heart’s electrical depolarization. In conditions like severe pericardial effusion, end-stage dilated cardiomyopathy, profound hypovolemia, or hypothermia, the heart’s mechanical and electrical forces are drastically diminished. The electrical signal reaching the skin surface is simply too faint for the amplifier to distinguish from background noise, resulting in an isoelectric (flat) line.
- High Skin-Electrode Impedance: The electrical signal must travel from the heart, through body tissues and fluids, to your electrode pads. Critically ill patients often have poor peripheral perfusion, subcutaneous edema, severe dehydration, or cool extremities. This creates high electrical resistance (impedance), scattering and weakening the signal before it reaches the electrode.
- Increased Environmental “Noise”: ICU patients are surrounded by sources of electromagnetic interference—ventilators, infusion pumps, fluid warmers. Furthermore, muscle tremor, shivering, or patient movement adds myoelectric “noise.” This noise can swamp an already low-voltage cardiac signal, causing the device to reject the trace.
Your Action Plan: Securing the Signal in Critical Care
When you encounter a flat line on a patient with a palpable pulse, follow this systematic protocol:
Step 1: Verify Your System
First, perform a quick system check. Unplug the cable from the electrode pads. Firmly apply your thumbs to the two metal plates of the cable connector separately. You should see a clear, clean ECG signal appear on the screen from your own cardiac rhythm. This simple, 10-second test confirms that the CardioBird device, cable, and software are functioning perfectly. It immediately rules out a technical fault and redirects your focus to the patient.
Step 2: Optimize the Patient’s Physiological State
With the system verified, turn your attention to the patient. Address reversible physiological factors that block signal transmission. For a hypothermic patient, initiate gentle warming. If indicated, use judicious fluid therapy to improve peripheral perfusion. Ensure the patient’s limbs are comfortably extended, not tightly flexed, to create a better electrical pathway.
Step 3: Master the Electrode-Skin Interface
This is the most critical clinical step you control, where 80% of issues are resolved.
- Site Preparation: Ensure proper skin-electrode contact by parting the hair. Clean the skin with alcohol, and if necessary, vigorously abrade the superficial skin layer (stratum corneum) with dry gauze. This dramatically reduces electrical impedance.
- Use Excellent Conduction: Apply a generous amount of high-quality ECG gel or ultrasound gel to the electrodes and the prepped skin. For long-term ICU monitoring, consider using adhesive ECG electrodes or liquid electrode gel for superior, stable contact.
- Explore Alternative Placements: move the electrodes from extremities (e.g. paws) towards the source (i.e. the heart). If limb placements fail, try mudflap placement (electrodes in the axillary region) or the chest placement. These can bypass areas of localized edema or poor perfusion.
By first understanding the physiology that masks the signal and then applying this structured approach, you can reliably secure an ECG on your most critical patients. This allows you to leverage CardioBird’s AI for continuous, life-saving monitoring when it is needed most.
Dealing with complex ICU cases? You’re not alone. Share your experiences and solutions with our global community of CardioBird users.

