The Turning Point: Real-World Stories Where an ECG Changed Everything – Case 3: Seizure vs. Syncope
Welcome back to our series, “The Turning Point,” where we spotlight real cases from your colleagues demonstrating how an ECG can dramatically alter a patient’s diagnostic path. This edition tackles one of the most challenging clinical dilemmas: distinguishing between a seizure and cardiac syncope.
The Patient: An 8-year-old Boxer with a history of two recent “collapse” episodes at home.
The Presenting Signs: According to the owner, the dog would suddenly collapse, become stiff, and make paddling motions for approximately 30 seconds before slowly recovering. The episodes were brief and the dog returned to normal shortly after. The physical and neurological exams in the clinic were entirely unremarkable.
The Turning Point – The Diagnostic ECG: The primary rule-outs were idiopathic epilepsy versus cardiac syncope. While the description leaned toward a seizure, the breed (a Boxer) raised a strong suspicion for arrhythmogenic right ventricular cardiomyopathy (ARVC). The veterinarian performed a CardioBird ECG. The trace revealed something critical: frequent, multiform ventricular premature complexes (VPCs) and a short run of ventricular tachycardia.
ECG Findings & Critical Difference:
This finding was the definitive “turning point.” While no arrhythmia was captured during an actual collapse event, the presence of significant ventricular ectopy in a Boxer is highly specific for underlying ARVC. This provided objective evidence that the “collapse” episodes were far more likely to be syncope caused by a transient, life-threatening arrhythmia, rather than a primary seizure disorder.
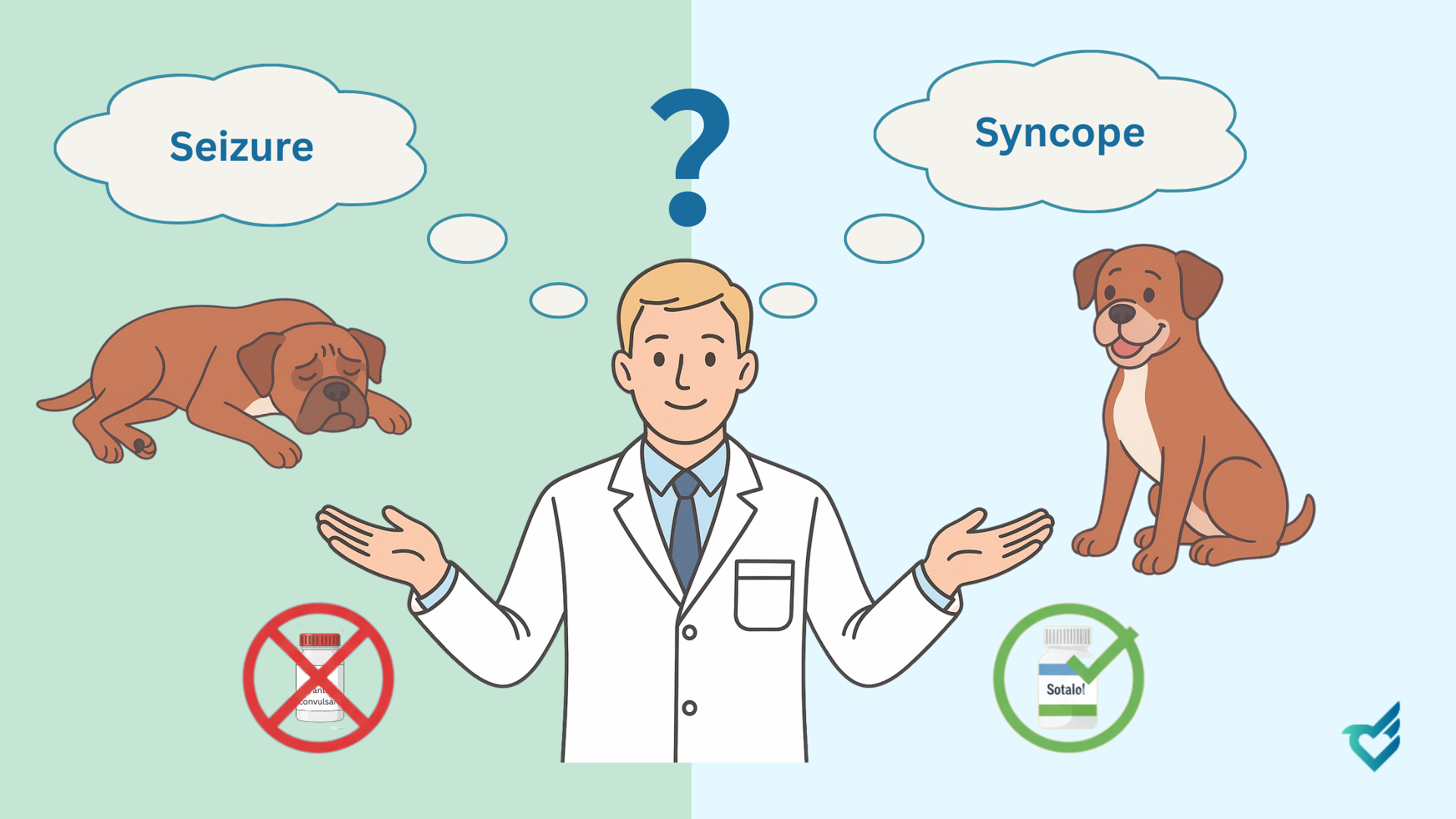
This ECG finding completely redirected treatment. Instead of starting anticonvulsant therapy, the diagnosis was cardiac. The patient was started on an anti-arrhythmic medication (Sotalol) and had a 24-hour Holter monitor scheduled to fully assess the arrhythmia burden. The owner was counseled on the nature of the disease and the critical importance of treatment, fundamentally changing the long-term management and prognosis.
Your Takeaway:
This case reinforces a critical rule in managing collapse episodes:
- An ECG is Mandatory in Every Case of Collapse: Regardless of how “classically” an episode sounds like a seizure, an ECG is a non-negotiable part of the workup. The clinical signs of syncope and seizure can be nearly identical.
- Breed Matters, But Evidence Rules: While breed predispositions (like Boxers and ARVC) should raise suspicion, the ECG provides the objective data needed to make a definitive call.
- Capture the Electrical Substrate: You may not capture an arrhythmia during the event itself, but finding significant VPCs or other arrhythmias in the inter-crisis period provides the “smoking gun” for an underlying cardiac cause.
By making an ECG the first-line test for any collapse, you move beyond guesswork. You are part of a global community using technology to uncover the hidden truth, ensuring patients receive the correct—and potentially life-saving—treatment from the very beginning.
Have a “Turning Point” case of your own? We’d love to feature it. Share your story with us.
