The Turning Point: Real-World Stories Where an ECG Changed Everything – Case 2: The GDV Patient

Welcome back to our series, “The Turning Point,” where we spotlight real-world cases from your colleagues that demonstrate how an ECG can dramatically alter a patient’s outcome. This edition focuses on a common emergency where ECG monitoring is crucial: Gastric Dilatation and Volvulus (GDV).
The Patient: A 6-year-old male German Shepherd presenting for acute abdominal distension and non-productive retching.
The Presenting Signs: Classic GDV presentation: anxious, tachycardic, with a painful, tympanic abdomen. The primary focus was immediate stabilization and preparation for surgery.
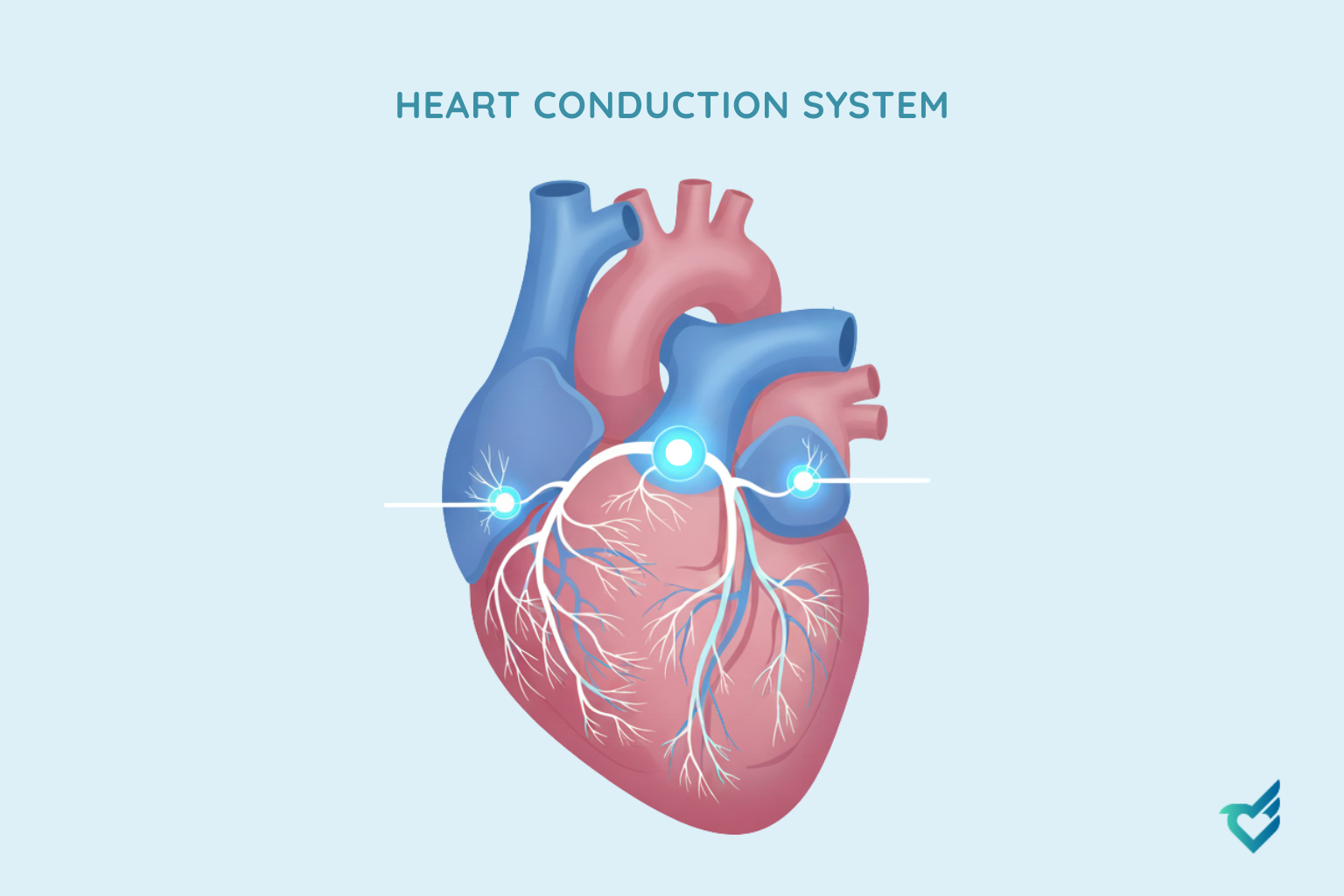
The Turning Point – The Emergency ECG: While placing an IV catheter, the team performed a rapid CardioBird ECG. Beyond the expected sinus tachycardia, the trace revealed something more concerning: frequent, multifocal Ventricular Premature Complexes (VPCs). These indicated significant myocardial irritability, a known complication of GDV.
ECG Findings & Critical Difference:
In GDV, cardiac arrhythmias are common and potentially fatal. They result from myocardial hypoxia, electrolyte imbalances, and the release of cardiotoxic substances. In this case, the ECG provided an immediate, objective assessment of the heart’s electrical stability before anesthesia.
This “turning point” ECG directly altered the anesthetic and medical protocol. Instead of rushing directly to surgery, the team initiated intravenous lidocaine to suppress the life-threatening arrhythmia. Continuous ECG monitoring with CardioBird allowed them to titrate the lidocaine drip to effect, ensuring the heart was in a more stable rhythm before and during induction. This proactive management significantly reduced the risk of cardiac arrest under anesthesia.
Your Takeaway:
This case reinforces critical protocols for managing the GDV patient, especially in high-risk breeds like the German Shepherd:
- ECG is Non-Negotiable in Triage: An ECG should be part of the initial stabilization workup for every GDV case, right alongside IV catheter placement and radiographs.
- Look Beyond Heart Rate: Don’t just count beats. Actively screen for ventricular arrhythmias (VPCs, ventricular tachycardia), which are common and may require specific treatment before anesthesia.
- Let ECG Guide Stabilization: The presence of significant arrhythmias is a signal to optimize the patient medically before anesthesia. This includes anti-arrhythmic therapy and correcting electrolyte abnormalities, turning a high-risk induction into a controlled one.
By making rapid ECG interpretation a standard part of your emergency protocol, you move from reactive to proactive care. You are part of a global community using technology to make critical decisions with confidence, ensuring the best possible outcome for your most vulnerable patients.
Have a “Turning Point” case of your own? We’d love to feature it. Share your story with us.