The ECG Decoded: A Veterinarian’s Guide to the Heart’s Rhythm: Part 3: Interpreting Chamber Enlargement and the Origins of Arrhythmias
Estimated reading time: 3.27 minutes
Welcome back to our series, The ECG Decoded: A Veterinarian’s Guide to the Heart’s Rhythm. We’ve built the electrical foundation and decoded the normal tracing. Now, we venture into the abnormal. This installment focuses on two critical concepts: how the ECG reveals structural heart changes and the fundamental mechanisms that cause rhythm disturbances. We’ll also address a common and crucial question: why can an ECG be normal in a patient with serious structural heart disease?
When the Heart Remodels: ECG Clues to Chamber Enlargement
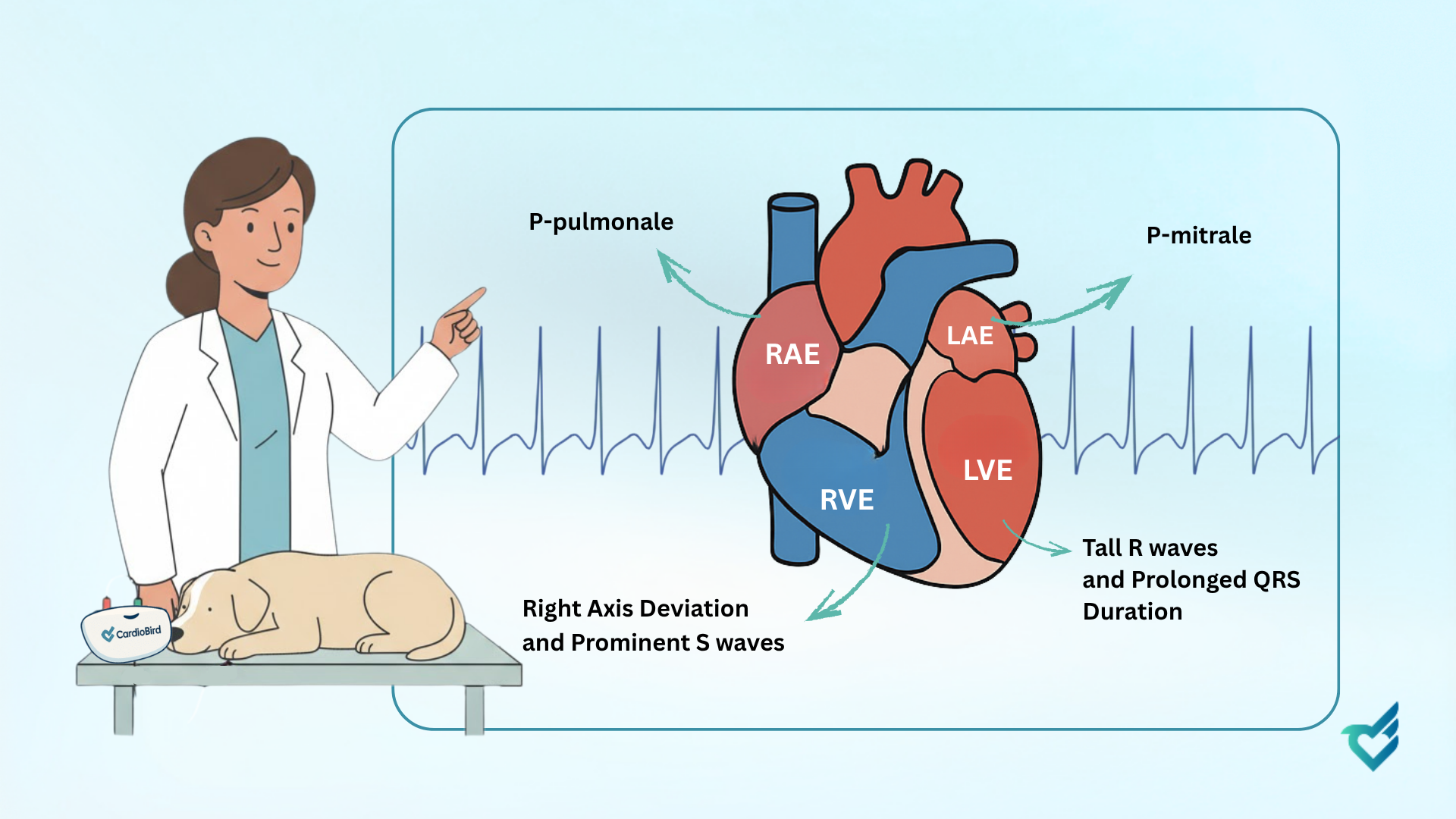
Chronic pressure or volume overload leads to hypertrophy or dilation, collectively termed chamber enlargement. This structural remodeling alters the heart’s electrical pathway, producing predictable changes. Recognizing these patterns is key to identifying underlying disease.
- Left Atrial Enlargement (LAE)
LAE is often a consequence of mitral valve disease. The enlarged atrium delays electrical conduction.
-
- ECG Hallmark: A wide and notched P wave, or P-mitrale.
- Left Ventricular Enlargement (LVE)
LVE results from pressure overload (e.g., systemic hypertension) or volume overload (e.g., patent ductus arteriosus). The increased muscle mass generates larger electrical forces.
-
- ECG Hallmarks: Increased QRS Amplitude (tall R waves) and Prolonged QRS Duration.
- Right Atrial Enlargement (RAE)
RAE is commonly seen with pulmonary hypertension or tricuspid valve disease.
-
- ECG Hallmark: A tall, pointed P wave, or P-pulmonale.
- Right Ventricular Enlargement (RVE)
RVE occurs with pressure overload on the right heart (e.g., severe heartworm disease).
-
- ECG Hallmarks: Right Axis Deviation and prominent S waves.
Why a Normal ECG Doesn’t Rule Out Structural Disease
A common question from clinicians is why a pet with a loud murmur or even echocardiogram-confirmed disease can have a “normal” ECG. The answer is fundamental: the ECG is an electrical report, not a structural one.
It can only detect problems that alter the heart’s electrical activity. Significant mechanical dysfunction, such as severe valvular regurgitation or myocardial failure, can exist without causing sufficient chamber enlargement or conduction delay to cross the ECG’s detection threshold. The ECG is excellent for diagnosing arrhythmias and significant enlargement, but it cannot assess contractility, valve function, or hemodynamic severity. This is why the ECG and echocardiogram are complementary, not redundant, tests.
Why Rhythms Go Wrong: The Pathogenesis of Arrhythmias
Arrhythmias arise from disturbances in the heart’s electrical properties: automaticity, triggered activity, or re-entry.
- Disorders of Automaticity
This occurs when a cell or group of cells outside the SA node fires faster, or when the SA node itself becomes dysfunctional.
-
- Enhanced Automaticity: A secondary pacemaker site speeds up, leading to atrial tachycardia.
- Depressed Automaticity: The SA node fails, resulting in sinus arrest.
- Triggered Activity
These arrhythmias are initiated by afterdepolarizations—abnormal oscillations that occur after an action potential.
-
- Early Afterdepolarizations (EADs): Occur during repolarization and are associated with a prolonged QT interval.
- Delayed Afterdepolarizations (DADs): Occur after repolarization and are caused by calcium overload (e.g., digoxin toxicity).
- Re-entry (Reentrant Tachycardias)
This is the most common mechanism for paroxysmal tachycardias. A single impulse travels continuously around a circuit, exciting the heart at a rapid rate. This is the typical mechanism for many supraventricular tachycardias.
A Practical Classification
For the clinician, a simple framework helps:
- Site of Origin: Supraventricular vs. Ventricular.
- Heart Rate: Bradyarrhythmia vs. Tachyarrhythmia.
This combination gives you a powerful starting point for diagnosis and management.
At CardioBird, our AI is engineered to recognize both rhythm abnormalities and the subtle patterns of chamber enlargement. We translate complex electrophysiology into clear, prioritized findings, empowering you to connect the dots between structure and electricity. We also provide context, helping you understand the limitations of a single test and the power of integrating ECG data with the full clinical picture.
In our next issue, we will delve into the specific diagnosis and management of bradyarrhythmias and conduction disturbances.
The CardioBird Team
